What is Fungal Acne [Is it Acne?]
What is Fungal Acne?
Fungal acne, often referred to as pityrosporum folliculitis or Malassezia folliculitis, is a type of skin infection that happens in your hair follicles due to an overgrowth of yeast called Malassezia. This yeast is naturally present on your skin, but when it overgrows, it can cause irritation and lead to the formation of bumps that resemble acne.
Unlike regular acne, which occurs when pores become clogged with oil, dead skin cells, and bacteria, fungal acne is caused by a fungal infection. It usually appears as small, red or flesh-colored bumps that are often itchy, especially on the chest, back, or forehead. The key difference is that while traditional acne is linked to clogged pores, fungal acne results from a microbial imbalance, where the yeast overpowers the skin’s natural defenses. So, while it looks like acne, it’s actually a fungal issue that requires a different approach to treatment.
How to Recognize Fungal Acne vs Regular Acne
Fungal acne can be tricky to identify because it often looks similar to regular acne, but there are some key differences that can help you tell them apart.
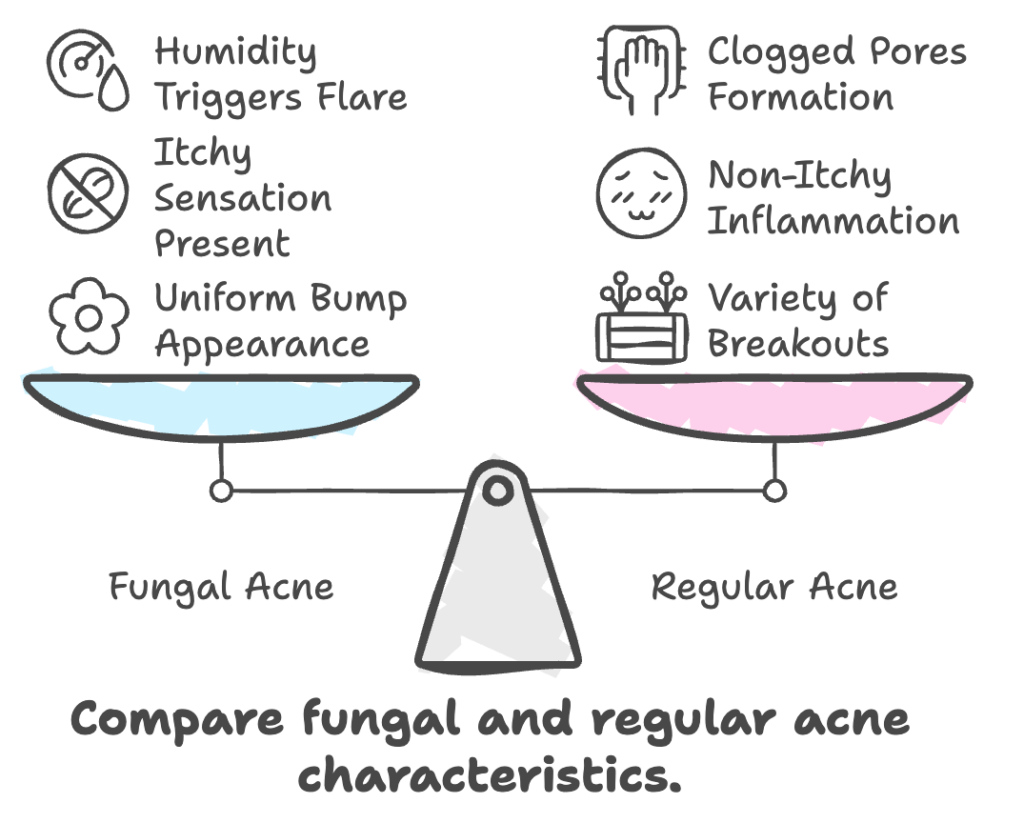
Fungal Acne:
- Appears as small, uniform bumps or a rash, usually on the forehead, cheeks, upper back, chest, and shoulders.
- The bumps tend to be the same size and may have a red ring around them.
- It’s often itchy and uncomfortable.
- Fungal acne is more likely to flare up in humid conditions, after sweating, or from wearing tight clothing or shaving.
Regular Acne:
- Typically involves more varied types of breakouts, such as blackheads, whiteheads, pustules, or cysts.
- It’s not usually itchy.
- Acne tends to form in clogged pores and can appear anywhere on the face, chest, or back, with breakouts in different stages of development.
So, while both conditions might look similar at first, the uniformity of the bumps, the itchiness, and the trigger factors like sweat or tight clothing are signs that you might be dealing with fungal acne. Regular acne, on the other hand, is more about blocked pores and can come in different forms, such as pimples or cysts.
Treatment for Fungal Acne
Treating fungal acne is different from regular acne, so it’s important to know what works best for this condition.
1. Antifungal Treatments:
Since fungal acne is caused by an overgrowth of yeast, typical over-the-counter acne treatments (like benzoyl peroxide or salicylic acid) won’t be effective. Instead, antifungal treatments are needed. These can be:
- Topical Antifungal Creams: Products like ketoconazole or clotrimazole are commonly used to treat fungal acne. These creams are applied directly to the affected areas.
- Oral Antifungal Medications: For more severe cases, oral antifungal medications like fluconazole might be prescribed by a doctor.
2. Professional Guidance:
It’s essential to consult with a dermatologist for a proper diagnosis. They can help determine if you’re dealing with fungal acne or another skin condition and recommend the right antifungal treatment for your specific case.
Fungal acne requires a different approach than regular acne, and getting the right treatment is key to clearing it up effectively. If you’re unsure, a dermatologist can guide you toward the best antifungal regimen for your skin.
Home Prevention Tips for Fungal Acne
Preventing fungal acne is all about keeping your skin in a balanced state and avoiding conditions that promote yeast overgrowth. Here are some helpful tips.
1. Keep Skin Clean and Dry:
After sweating, whether from exercise or heat, make sure to shower and dry your skin thoroughly. Yeast thrives in warm, moist environments, so keeping your skin dry helps prevent fungal growth.
2. Wear Breathable, Loose Clothing:
Opt for loose-fitting clothes made of natural fabrics like cotton, which allow your skin to breathe. Tight clothing or synthetic fabrics can trap moisture and create a breeding ground for yeast.
3. Avoid Unclean Hot Tubs and Pools:
Hot tubs and swimming pools that aren’t properly maintained can harbor bacteria and fungi. If you’re using them, make sure they are well-maintained and regularly cleaned to reduce the risk of fungal infections.
4. Use Selenium Sulfide Shampoo:
Selenium sulfide is an antifungal ingredient commonly found in dandruff shampoos. You can use it as a body wash once a week to help combat fungal acne. It can help reduce yeast on your skin, preventing overgrowth.
5. Natural Remedies with Caution:
Some people use tea tree oil as a natural antifungal remedy. While it has antifungal properties, it’s important to use it with caution, as it can be irritating to the skin and potentially neurotoxic if not diluted properly.
By incorporating these preventive measures into your routine, you can help minimize the risk of fungal acne and keep your skin healthier.
When to See a Dermatologist

If you’re unsure whether you’re dealing with fungal acne or regular acne, or if your current treatments aren’t working, it’s important to consult a dermatologist. They can provide a proper diagnosis and recommend the right treatment for your skin. Here are a few signs that it might be time to see a dermatologist:
1. Persistent or Worsening Symptoms:
If the bumps or rash don’t improve after trying over-the-counter treatments or if they continue to spread, a dermatologist can help determine whether it’s fungal acne or another skin condition.
2. Unclear Diagnosis:
If you’re uncertain whether your breakouts are fungal acne or regular acne, a dermatologist can perform tests to pinpoint the cause and ensure you’re treating the right condition.
3. Severe or Painful Breakouts:
If you experience pain, swelling, or large cyst-like bumps, it’s time to get professional help. This could indicate a more severe case or another type of skin issue that needs targeted treatment.
4. Difficulty Finding the Right Treatment:
Over-the-counter acne treatments typically won’t work for fungal acne, so if you’re struggling to find the right solution, a dermatologist can prescribe antifungal medications or suggest alternative treatments.













Post Comment